100% Pass-Through Approach
Unlike traditional models, we pass all discounts and rebates through to clients
For over 20 years, we have led the way as a transparent, pass-through PBM. It is our legacy.
We work on behalf of our clients to further purchasing efficiencies and deliver all rebates and discounts directly to them. Clients realize cost savings within the first year, through lowered total drug spend and lower per member per month (PMPM) expense.
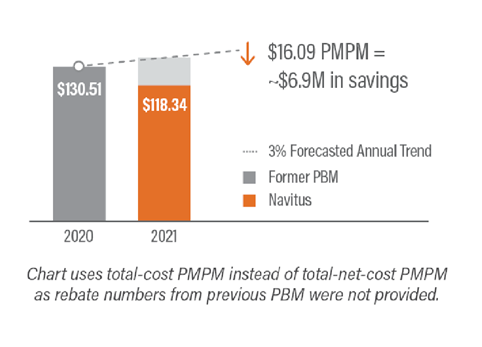
Savings Realized in Year 1
By removing spread pricing and implementing formulary management approaches, a new health plan client with 35,000 covered members realized nearly $7M in first-year savings. This equated to a 9% reduction in PMPM cost compared to forecasted PMPM cost with the prior PBM.
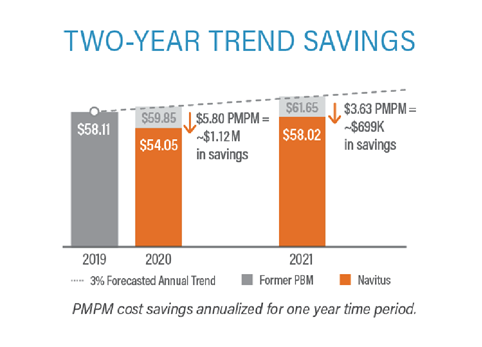
Continued Savings Year-Over-Year
Our data indicates that Navitus clients realize savings past Year 1. A national employer group with more than 16,000 covered members realized savings of $1.1M in the first year and almost $700k of additional savings in year two.
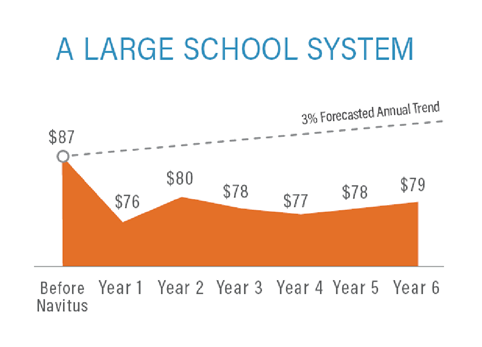
6-Year Cumulative Savings
Savings can continue, even with the pressure of incremental cost increases. Clients continue to see a PMPM cost trend below that of the previous PBM even after six years with Navitus.
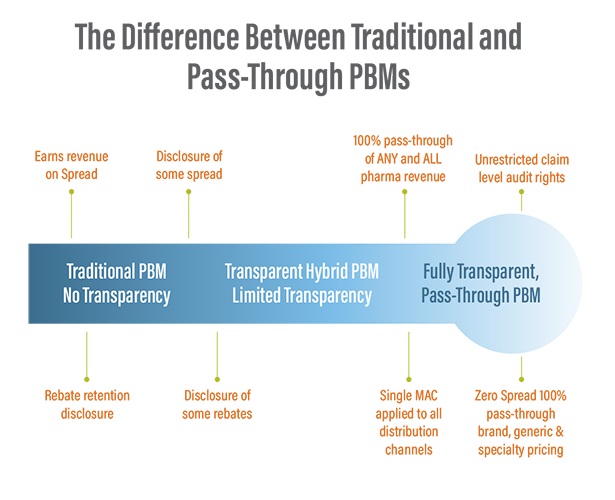
How Transparent is Your PBM?
In traditional models, a PBM will create and take margin (“spread”) between what it pays the pharmacy and what it bills the payor client when a member receives a prescription medication under his or her benefit. This margin creation also occurs within the collection and distribution of rebates and discounts, where the PBM collects more rebates and discounts than it passes along to the payor.
Payors choose Navitus as their PBM when they recognize the value of a no-spread, 100% pass-through approach. They realize the value of true partnership and alignment toward the goal of removing, not shifting, cost from the drug supply chain.